We talk about it all the time. We know we’re not supposed to have too much of it, and we know that it has to do with the foods we eat. But for many of us, that’s about as far as our understanding of cholesterol goes. In this article, we’ll cover the basic biology of cholesterol, the good and bad aspects of cholesterol for our health, the difference between “good” and “bad” cholesterol, and risk factors for having too much of it circulating in our blood.
Cholesterol basics
The very word “cholesterol” has negative connotations for most people. Yet without it, we would die. You have this lipid—a waxy, fat-soluble molecule—in every cell of your body, and that’s a good thing, since cholesterol functions in a variety of beneficial ways. It supports the integrity of cells, helps convert sunlight into vitamin D, and is a building-block for sexual hormones.
Your liver produces all the cholesterol you need to support those functions. Because cholesterol is destined to reach every cell of your body, it travels through your blood vessels to get there. Excess cholesterol that isn’t absorbed by the cells finds its way back to the liver, where it is either converted into bile salts or destroyed and expelled as waste.
That’s the good side of cholesterol. The bad side comes in when we eat the wrong foods and prompt the liver to produce more cholesterol than is necessary. Among American adults, some 95 million have excessive levels of cholesterol. When there’s too much cholesterol in circulation, it starts to build up on the inner linings of the arteries, a condition known as atherosclerosis. As it accumulates, it starts to restrict blood flow through the artery. Plaques of it form inside the artery and eventually calcify, causing a partial or total blockage. When a plaque ruptures, the substances bound up in the plaque break free, causing a bloood clot that can result in a stroke or heart attack.
Good and bad cholesterol (HDL vs LDL)
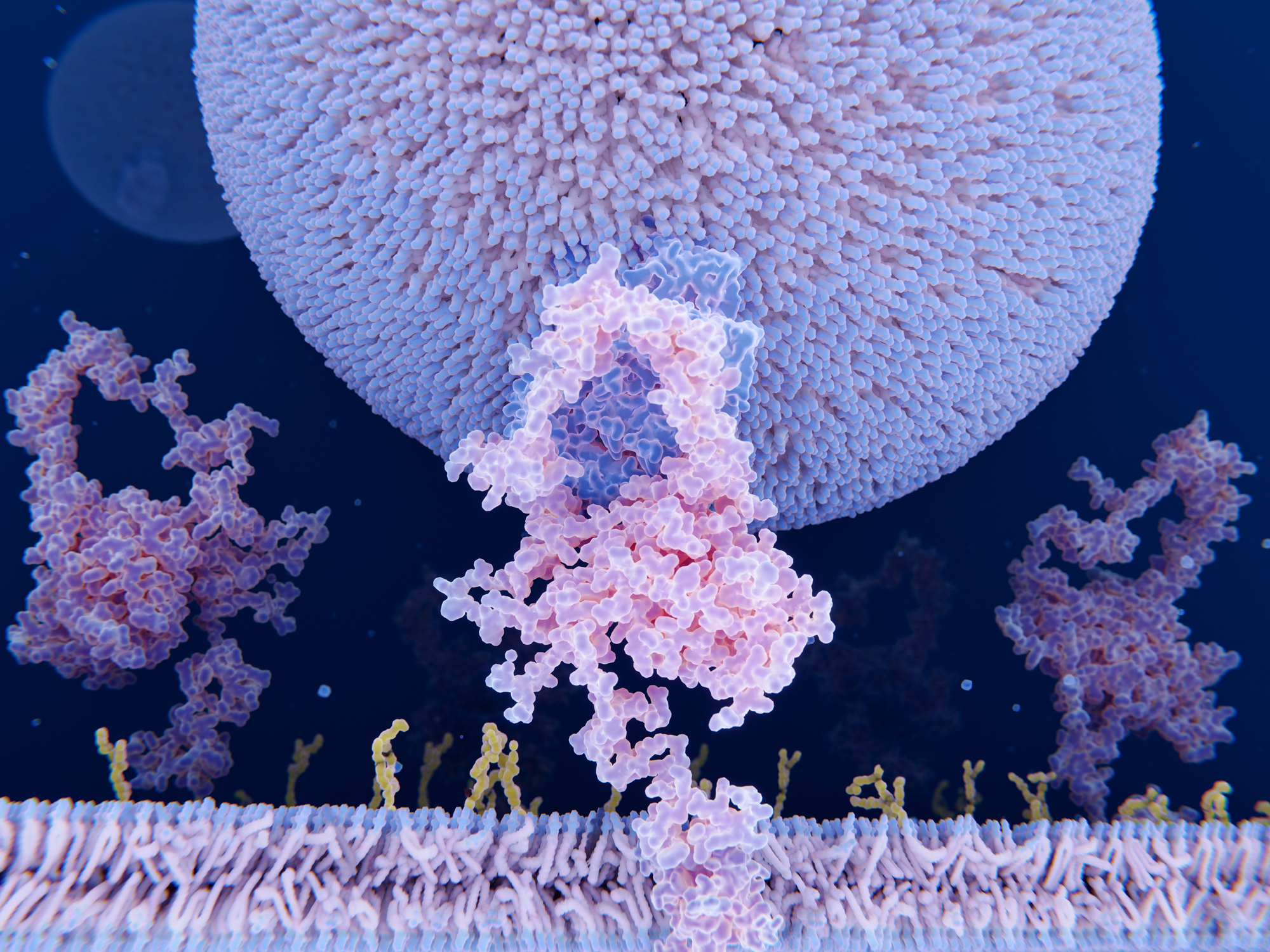
Cholesterol doesn’t just swim freely in the bloodstream. It rides along on spherical substances called lipoproteins. Some lipoproteins are very dense and others more diffuse. Low-density lipoprotein is known as LDL cholesterol (Even though technically a lipoprotein consists both of protein and cholesterol, we refer to it as a form of cholesterol). LDL is commonly called “bad” cholesterol because as we accumulate more of it, our cardiovascular risk increases. High-density lipoprotein is called HDL, the “good” cholesterol. That’s because it doesn’t accumulate on our arterial walls the way LDL does. In fact, as it travels through our bloodstreams, it collects LDL and carries it back to the liver to be disposed of. Experts estimate that 25-30% of our LDL cholesterol is removed in this way by HDL cholesterol.
Another important type of lipids is triglycerides. When you eat excess calories, your body converts them into triglycerides, and high triglyceride levels are closely associated with negative cardiovascular outcomes.
When you get your cholesterol levels checked, your doctor will look at your levels of HDL, LDL, triglycerides and perhaps other lipids. Obviously, you’ll want to see that you have high levels of HDL and low levels of LDL, and that you’re keeping your triglycerides as low as possible. One of the parameters often found on lipid panels is “total cholesterol.” Most doctors place less importance on total cholesterol per se and more on the ratio of total cholesterol to HDL. A ratio of 5 or lower is usually considered acceptable.
Food and cholesterol
A common misconception is that the primary way in which we cause our LDL levels to rise is by eating foods that are high in cholesterol. While consumption of cholesterol-rich foods may have a modest impact on circulating cholesterol, experts no longer think of this as the key mechanism. Instead, our lipid profile worsens when we consume saturated fats (from animal-derived foods), excess calories, and sugar.
An uneven playing field
It would be nice to think that each of us had a similar baseline whereby our livers produced exactly the right amount of cholesterol, and that our bodies all responded similarly to the foods we eat. Unfortunately, that’s not the case. High cholesterol tends to run in families, and even within the same family, individual members may produce more natural cholesterol and see different results when they eat the same foods.
The key genetic variant in play is called APoE4, or apolipoprotein E4. People with that variant tend to develop higher levels of LDL cholesterol. Some people’s genetic deck is so stacked against them that they develop a condition called familial hypercholesterolemia, which usually causes high cholesterol at a very young age.
Is high cholesterol reversible?
Yes! To date, there’s no magic medicine that can “fix” your cholesterol levels, and someone with a family history of high cholesterol might always struggle with keeping their cholesterol at bay…but genetics is not destiny, since we now have multiple ways of mitigating whatever risk we might have inherited. Eating a diet low in saturated fats, high in fiber, and low in sugar is one way to give ourselves a leg up. Abstaining from smoking and drinking is another, as is getting enough sleep and exercise. And we now have several effective, well tolerated drugs for managing cholesterol.
The important thing is that you learn what your cholesterol levels are and, if they’re high, take proactive steps to manage them. Accumulated cholesterol causes damage to the blood vessels, so you want to act quickly to improve your numbers. The longer you wait, the less likely you’ll be able to prevent a bad outcome.