Most people have heard of amyloid plaque and understand that it has something to do with Alzheimer’s disease. But what is it exactly, and what role does it play in the development and symptoms of dementia? Researchers are learning more and more about this substance and developing an ever-more-sophisticated understanding of the part it plays in Alzheimer’s.
Amyloid Precursor Protein
To understand amyloid and the biology of Alzheimer’s, it’s important to start with a protein called amyloid precursor protein (APP). APP occurs naturally in brain cells (neurons), helping them to grow, maintain stasis, and create new nerve paths which help different parts of the brain stay connected. Sometimes, for reasons researchers still don’t understand, lengths of APP get cut up into smaller strands, enzymes known collectively as secretases. One of these, called beta amyloid, is particularly problematic. It’s sticky, and its short pieces are prone to clumping together. When beta amyloid clusters form, we call them amyloid plaques.
Those plaques are one of the hallmarks of Alzheimer’s disease. A major theory of Alzheimer’s, called the amyloid hypothesis, is that the formation of plaques is a cause of the disease. As the amyloid displaces or kills healthy nerve cells and accumulates between them, disrupting memory and thinking, parts of the brain begin to fail, usually starting with the hippocampus, sometimes called the memory center. Yet autopsies have revealed that plenty of people have amyloid plaque in their brains without ever developing dementia, so it is not as simple as pointing to amyloid plaques as a sufficient cause of the disease.
Tau Protein
Amyloid is one of two proteins present in the brain which appear to play key roles in Alzheimer’s. The second such protein is called tau and, like APP, it’s normally beneficial. In a healthy brain, tau forms microscopic tubes in brain cells which transport communication signals. But in Alzheimer’s, tau become corrupted, forming twisted strands called neurofibrillary tangles. Those tangles disrupt communication signals as well as the cell’s ability to repair itself. Neurons affected by tau tangles will eventually die…and unfortunately, neurofibrillary tangles spread from one cell to another, with their damage sweeping over entire parts of the brain. Tau tangles usually first form in the entorhinal cortex, an area of the brain closely associated with memory, and move on from there toward the brain’s language centers.
It may be that amyloid plaques and neurofibrillary tangles work in concert as drivers of Alzheimer’s disease, which is why researchers often speak of them together.
Inflammation’s Role in Alzheimer’s
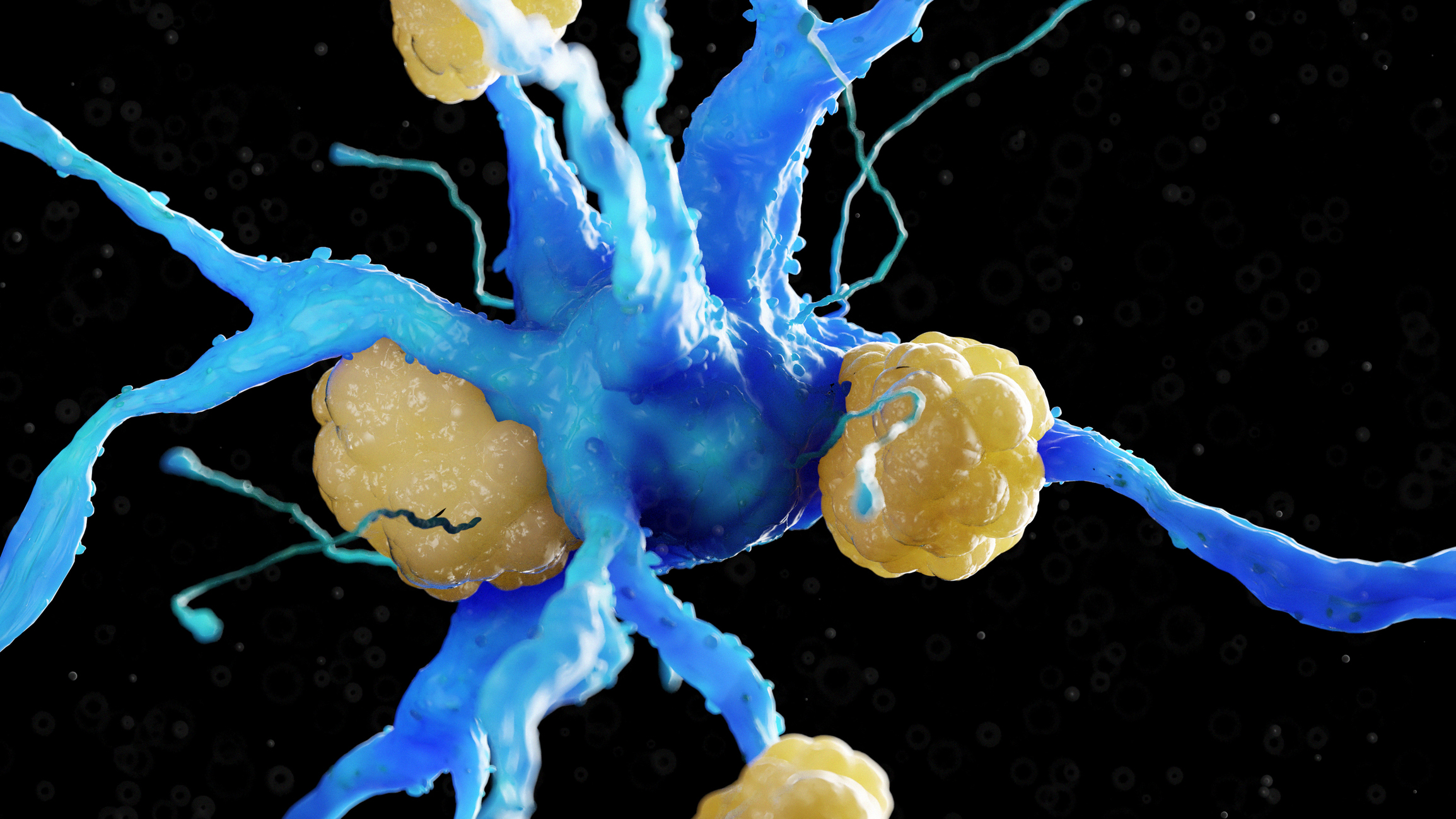
Some researchers are now exploring the possibility that much of the neuronal damage in Alzheimer’s is caused not by the mere presence of amyloid plaque, but by the body’s immune response to those plaques. In our brains, we have special immune cells called microglia whose job it is to attack and destroy harmful substances. When amyloid plaques or damaged tau appear in brain cells, the microglia, detecting a serious threat, go into action. The result is a kind of scorched-earth campaign of inflammation, with considerable “collateral damage” in the form of healthy brain cells that get destroyed by the body’s own defenses.
Detecting Amyloid
Until recently, doctors couldn’t be certain how much amyloid was present in a person’s brain until after death, when an autopsy was performed. Today, we have multiple ways of detecting amyloid while the person is still alive.
One method of detecting amyloid is via a positron emission tomography (PET) scan using a compound that binds to the amyloid plaque and shows up in imaging. Because of their expense and difficulty, these amyloid PET scans are currently not used to identify people who might have Alzheimer’s. Instead, they help physicians diagnose which type of dementia a person has.
Doctors also can detect amyloid and tau by sampling a person’s cerebrospinal fluid, but this requires a spinal tap (the insertion of a needle between two vertebrae in their lower back to withdraw fluid) and is therefore less desirable than other methods. In the fluid sample, doctors look for lower levels of a substance called beta-amyloid 42 and higher levels of tau to confirm the presence of plaques and tangles.
Researchers are striving to develop less-invasive and less-expensive methods of detection, including blood tests. One test already in use indicates how much beta-amyloid 42 and beta-amyloid 40 are circulating in the bloodstream, and thus how much of those substances is present in the brain. From that, doctors get a better idea of the risk of amyloid plaques in the brain and the risk of developing Alzheimer’s. However, the test cannot currently be used to make an Alzheimer’s diagnosis. But before much longer, we may see Alzheimer’s screening via blood biomarker tests become a routine part of wellness visits.
Amyloid Risk Factors
What causes brain plaques? As with so many things in medicine, researchers speak less about direct causes and more about risk factors, meaning possible contributors. The following factors have all been found to play a role in the presence of cerebral plaques:
- Defective genes. Mutations of three genes are connected to the corruptive process whereby amyloid precursor protein splits apart into beta-amyloid.
- Depression. Chronic negative thoughts have been associated with higher levels of plaque and tau in the brain.
- Air pollution. A 2024 study found that people with high exposure to particulate matter from traffic were about 90% more likely to have high levels of amyloid plaque.
- Head injuries. People without a history of head trauma are less likely than those who have been injured to have beta‑amyloid plaques in their brains.
- Disrupted sleep. It’s during deep sleep that the brain clears away harmful substances such as beta-amyloid and tau, so chronic sleep problems including insomnia and sleep apnea may contribute to the accumulation of those toxins.
- Poor gut health. Investigating the “gut/brain axis,” researchers have found that people with more amyloid and tau in their brains have lower levels of two anti-inflammatory gut bacteria known to have neuroprotective effects.
- Down Syndrome. People with Down Syndrome are very susceptible to Alzheimer’s. They have three copies of the chromosome on which appears the gene that produces abnormal amyloid precursor protein which breaks down into beta-amyloid to form plaques.
Can Amyloid Be Cleared Away?
Over the past few years, new monoclonal antibody drugs have come onto the market which work by spurring an immune response that wipes out beta-amyloid. They have in fact proven effective in terms of reducing the amount of beta-amyloid in the brain, but the resulting effect on cognition has been disappointing. The drugs modestly slow the progression of Alzheimer’s but have a negligible positive effect on thinking and remembering.
The disappointing benefit of these drugs, despite their ability to clear away plaque, underscores the complexity of Alzheimer’s disease, suggesting that, while amyloid is important, it is only one part of the story, with much still to be learned. On the other hand, drugs currently in development that operate similarly have, in early trials, enjoyed greater success in slowing disease progression.